Bloodborne Pathogens: A Safety Guide
Jun 14th 2018
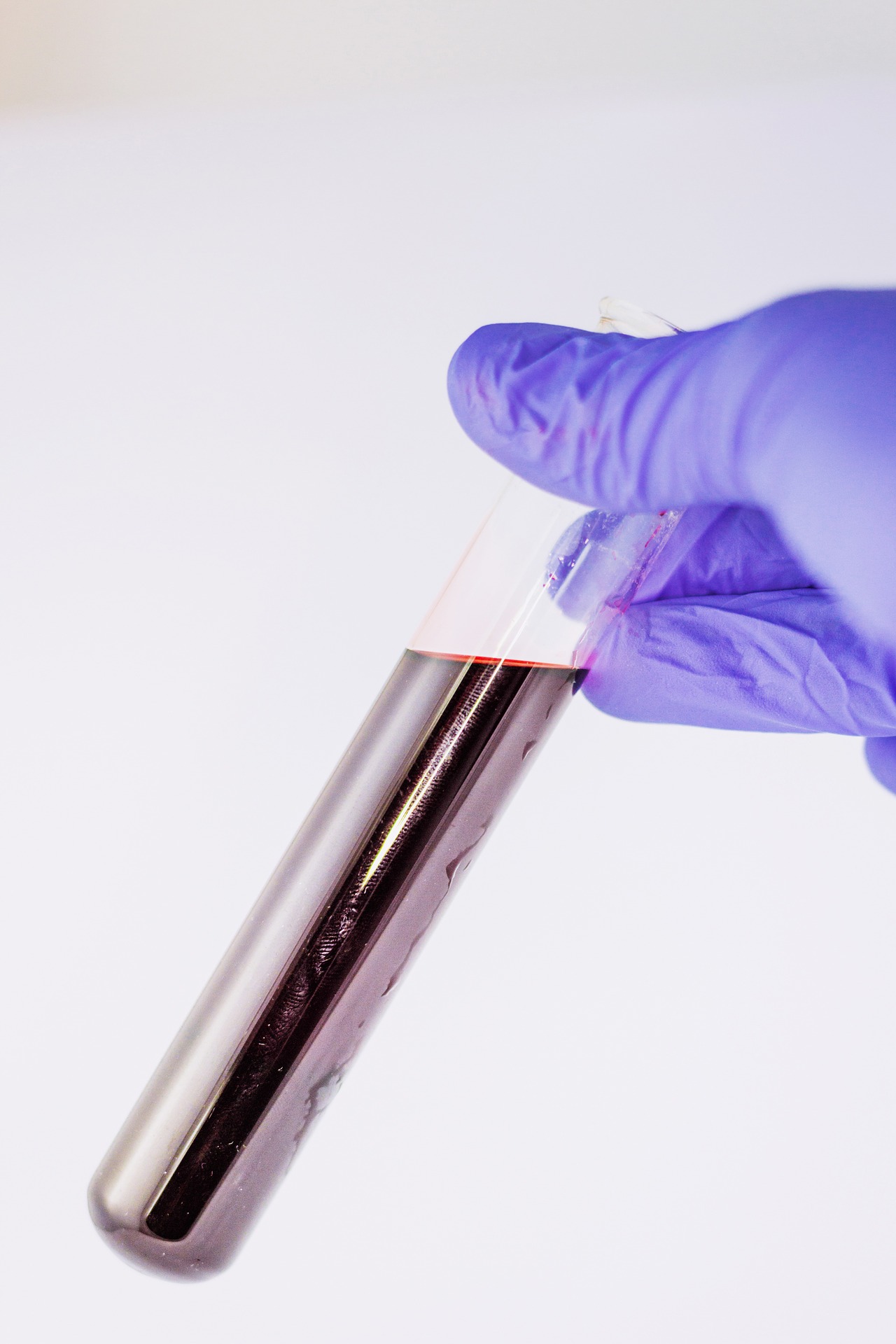
Bloodborne pathogens are microorganisms in blood that can cause diseases. Bloodborne pathogens can be transmitted through contact with infected blood and other bodily fluids. To prevent the spread of disease, an Exposure Control Program must be developed in compliance with OSHA standard 1910.1030.

ELEMENTS OF AN EXPOSURE CONTROL PROGRAM
OSHA standard 1910.1030 applies to every employee with the potential for occupational exposure to bloodborne pathogens. The plan must be written and readily accessible to all employees. Every employee covered by the standard must receive exposure control training at least once a year. An exposure control plan contains the following information:
- Program Administration
This section explains how the exposure control program is going to be administered. Administrative responsibilities must be named by job title and a brief description of responsibilities. For instance, this section will name the job title responsible for providing, maintaining, and disposing of personal protective equipment. Job titles and administrative descriptions must also be provided for training, evaluation, and recordkeeping.
- Determination of employee exposure
This section has a list of all job titles with the potential for exposure to bloodborne pathogens. This section should also contain the department name and the task carried out by the employee.
- Methods of exposure control
This section contains detailed information on the exposure control plan, engineering controls and best work practices, PPE and PPE maintenance, safe housekeeping instructions, safe laundry instructions, and required signs and labels. In short, this section lists all the ways that exposure to bloodborne pathogens are being controlled and lists the job title responsible for each action.
- Hepatitis B Vaccination information
Employers are required to provide Hepatitis B vaccinations free of charge to all employees who may be exposed to bloodborne pathogens. This section details the job titles responsible for educating employees about the risks of Hepatitis B and administering the vaccine. This section also details procedures for employees who choose to decline the vaccine.
- Recordkeeping
This section contains detailed information about what records are kept, for what purpose, and for how long. This includes training records, medical records, OSHA incident records, and a Sharps Injury Log.
- Exposure Procedures
This section details the steps to be taken in the event of an exposure. This includes documenting the exposure, including the time, place, source individual, and procedures to get the source individual and any exposed employees the appropriate medical testing.
- Exposure Evaluation
This section evaluates the circumstances surrounding the exposure and the measures taken to prevent another such instance from recurring. Procedures for recording injuries following an exposure are also contained in this section. The job title or department responsible for each task should be named.
- Information and training
This section details the topics that will be covered in training and names the department or job titles responsible for administering the training. It will also contain information on storing the training materials and making the Exposure Control Program accessible to employees.
BLOODBORNE PATHOGEN RISKS
The risks associated with bloodborne pathogens are serious. Exposure to pathogens could lead to disease, which can cause severe pain, discomfort, reduced quality of life, and even death. Special precautions and procedures must be developed for three pathogens: hepatitis B, hepatitis C, and the human immunodeficiency virus (AIDS).
HEPATITIS
Hepatitis B is a virus that infects the liver and causes inflammation. Hepatitis is a potentially life-threatening disease. Acute hepatitis B can occur if an uninfected person is exposed to the virus. In many cases, acute hepatitis goes away on its own. In some cases, the infection remains in the body and chronic hepatitis B develops. Complications of chronic hepatitis can include cirrhosis of the liver, liver cancer, and liver failure. Symptoms of hepatitis B include:
- Abdominal pain and vomiting
- Fever
- Fatigue
- Clay-colored bowel movements
- Joint pain
- Jaundice
It is important to note that some people experience no symptoms. A person can still be infectious to others even if they are not experiencing symptoms. Hepatitis B can survive for up to a week in dried blood.
Hepatitis B can be prevented through the hepatitis B vaccine. The vaccine is very effective with few adverse reactions. Employers are required to provide the hepatitis B vaccine free of charge to any employee who may be exposed to the virus. Employees have the right to refuse the vaccine, but they must sign a waiver that indicates their consent and an understanding of the risks they face from possible exposure. An employee who refuses the test can change their mind at any time.
Hepatitis C has many of the same symptoms as hepatitis B, including abdominal pain, vomiting, fever, fatigue and jaundice. Like hepatitis B, many people who have hepatitis C experience no symptoms. Relative to hepatitis B, hepatitis C has an increased risk for indirect exposure; it can survive in dried blood for up to three weeks. Acute hepatitis C develops into a chronic condition in about 75-85% of cases (https://www.cdc.gov/hepatitis/hcv/cfaq.htm). Like hepatitis B, hepatitis C can result in cirrhosis of the liver, liver cancer, and liver failure. There is not yet a vaccination available to hepatitis C.
HIV/AIDS
The human immunodeficiency virus (HIV) is the pathogen that causes acquired immunodeficiency syndrome (AIDS). Many people who contract HIV will not experience symptoms. Other people can experience the following symptoms in the early stages of the disease:
- Fever
- Nausea
- Swollen lymph nodes
- Fatigue
- Muscle aches
- Rash
There is no immunization or known cure available for HIV. If infected, drug therapies are available that can help patients manage their symptoms. Available drug therapies have also significantly decreased the overall death rate from HIV/AIDS.
CONTROLLING AN EXPOSURE
All bodily fluids should be treated as if they are potentially infectious. This attitude will help employees approach exposure incidents with the requisite caution.
Engineering and Work Controls
Engineering controls refer to the practice of removing or containing hazardous materials. This includes proper disposal containers for sharps or contaminated laundry.
Work controls refer to the way in which cleanup and medical tasks like first aid are performed. This includes wearing the appropriate personal protective equipment (PPE), which must be supplied by your employer. Disposal gloves and protective face masks are often used when working with potentially infected blood. In a first-aid situation, resuscitation masks and CPR barrier shields with one-way valves may be required. Infections can be transmitted through your eyes, nose, mouth, and broken skin, so effective PPE must protect these areas from exposure.
If there is a possibility of hand contact with blood or any other bodily fluid, disposable gloves must used.
Signs
Signs or labels are required for any container or object containing biohazardous materials. Compliant signs must have a fluorescent orange background, the universal biohazard symbol, and the word “biohazard” written on them. Approved red biohazard bags or containers that have the biohazard symbol on them do not require signs.

Zing Sign # 10053
Housekeeping
Safe housekeeping refers to the process of keeping your workplace clean, sanitary, and uncluttered. In relation to bloodborne pathogens, safe housekeeping has two main tasks. The first is to to prevent exposure incidents from occurring by minimizing clutter, sharp edges, and other hazards that may cause an accident. The second is to make sure an environment is properly cleaned and disinfected following an exposure incident.
Procedures must be in place to properly contain and dispose of regulated waste. Regulated waste is waste that requires special handling procedures. Any items containing blood or other potentially infectious materials are regulated waste. This includes blood, any towels or other items used to clean blood, and contaminated sharp objects.
We have mentioned that the proper PPE must be used when cleaning up blood or other potentially infectious materials. If cleaning up sharp objects, use forceps or some other mechanical means to gather the hazardous objects. Never use your hands to clean a sharp object, even if you are wearing gloves.
Once cleaned, infectious waste needs to be properly contained. Compliant containers must be leak-proof and clearly labeled as biohazardous.
Surfaces that are exposed to possibly infectious materials must be thoroughly disinfected to prevent indirect transmission of bloodborne pathogens. When using chemical disinfectants, wear the appropriate PPE. All reusable receptacles must be decontaminated regularly.
Potentially contaminated laundry must be handled carefully with gloves and placed in designated receptacles. Contaminated laundry should never be taken home by any employee.
Needlesticks
In 2001, OSHA published the Needlestick Safety and Prevention Act, which contained new additions to the exposure control plan and recommended new engineering controls to reflect advances in medical equipment. Updates included:
- Adopting and documenting the use of safe, effective devices that reflect the best medical technology, such as devices that reduce the use of needlesticks. This includes identifying which devices were considered for use, and the justification for the devices that were selected for use.
- Procedures for maintaining a needlestick and sharps injury log. These include, the type or brand of device involved in the injury, the department or work area in which the exposure occurred, and a description of the circumstances of the exposure event.
EXPOSURE AND TRANSMISSION

For a bloodborne pathogen to cause an infection or disease, four conditions must be met:
1. A pathogen must be present in an exposure to bodily fluids.
2. There must be an entry site for the pathogen (usually through a mucous membrane or broken skin)
3. The pathogen must enter the body in sufficient concentration to overwhelm immune response.
4. The affected person must have a susceptibility to the pathogen.
Exposure to potentially contaminated materials can occur directly or indirectly. Direct exposure means immediate contact with blood or other infectious materials. Indirect exposure means that infectious material is present on an intermediate object, such as a door handle or hard surface. In the workplace, bloodborne pathogens are transmitted primarily through mucous membranes, such as the eyes, ears, nose, and mouth; or through broken skin, such as cuts or scrapes. Wounds, such as a puncture by a sharp object, can also cause broken skin. Pathogens are not transmitted through casual contact like shaking hands. Sexual contact and sharing needles are also common ways of transmitting bloodborne pathogens.
If an exposure occurs, immediate action should be taken. If you suspect your eyes, mouth, or nose have been exposed, the affected area should be thoroughly flushed with running water. If you suspect an exposure through broken skin, thoroughly wash the affected area with soap and water. If soap and warm water is not available, use an alcohol-based hand sanitizer or antiseptic wipes to clean the affected and surrounding areas. If any potentially contaminated debris is present, it should be removed before applying the sanitizer.
Any clothing or PPE that is exposed to contaminated fluids must be placed in a compliant biohazard receptacle.
POST-EXPOSURE PROCEDURES
Reporting the Incident
If an exposure occurs, it must be reported as soon as possible to make sure exposed employees receive the medical attention they need. The follow-up of the incident includes recording the circumstances of the exposure and identifying the source individual. The source individual must have their blood tested to determine the risk posed to exposed employees, unless this is prohibited by state or local law.
Medical Evaluation and Follow-up
Any affected employee must be directed to a licensed health-care professional as soon as possible for a confidential medical evaluation and testing. The evaluation and testing must be provided free of charge. Any testing must be conducted by an accredited laboratory. Post-exposure prophylactic measures must be offered to the exposed worker according to the current recommendations of the U.S. Public Health Service.
CONCLUSION
Bloodborne pathogens can cause diseases that can severely lower an employee’s quality of life and even cause death. A rigorous safety plan can prevent serious exposure events from occurring and can help minimize risk and damage in the event of an accident. Developing a compliant bloodborne pathogen program is imperative and may save lives in your workplace. For more information on bloodborne pathogen safety, visit: https://www.osha.gov/pls/oshaweb/owadisp.show_doc...
